Translate:
All media inquiries , collaborations interviews, events call or email.
EN
Translate:
All media inquiries , collaborations interviews, events call or email.
EN
Signed in as:
filler@godaddy.com
Symptoms of Hyperemesis Gravidarum (HG)
Severe nausea and /or vomiting that you are unable to eat and drink or function.
▪︎Food aversions
Weight loss of 5% or more of Pre-pregnancy weight.
Decrease in urination ,Brown or orange urine.
Dehydration
Headaches
Confusion.
Hallucinations due to severe dehydration.
Fainting
Jaundice
Extreme fatigue
Low blood pressure.
Rapid heart rate.
Sweating and or chills
Body ache
Stomach pain severe,
burning pain in throat from vomiting/ throat raw due to extreme vomiting
Battery acid heartburn
Loss of skin elasticity
Anxiety/depression
Content nausea that affects everyday life.
unusual thoughts or behaviors.
Vomiting and unable to hold food or fluids down
Ketones in your urine.
Everything you drink or eat comes back up.
Unable to eat or drink due to severe nausea with vomiting or dry heaving take in any amount of food.
Anemia
With HG you can go from hot to cold, sweating and have the chills that can cause body odor (from rapid fat loss & ketosis)
Decreased urination.
Feeling pressure you have to pee and only pee a drop. -
Dehydration/ Malnourishment.
Dry, furry tongue. Cracked corners of lips or chapped cracked lips, that can bleed.
Excessive salivation you must spit out.
Extreme fatigue more than normal. -Fainting or dizziness combined -Gall bladder dysfunction -Hypersensitive gag reflex -Increased sense of smell( Like a hound dog) -Intolerance to motion/noise/light. -Ketosis. -Liver enzyme elevation. -Loss of skin elasticity. -Low blood pressure. -Overactive thyroid or -parathyroid. -Pale, waxy, dry skin. -Rapid heart rate. -Vitamin/electrolyte deficiency. -Vomiting of mucus, bile or blood.
Acute Morning Sickness

It’s all in our DNA. CVS and Hyperemesis Gravidarum is connected by a DNA mutation-called the RYR2 Factor much more research is needed as to why the Strong family are volunteer leaders for the HER Foundation. In 2016 this was groundbreaking research with UCLA .
The RYR2 gene, encoding a stress-induced calcium channel present in many neurons, was the only gene demonstrating a statistically significant difference in the proportion of conserved sequence variants among the groups. HG is triggered differently in each of us , this is why each treatment is not textbook.
A new study led by researchers at UCLA and published in the journal Nature Communications has identified two genes associated with Hyperemesis Gravidarum,( HG) whose cause has not been determined in previous studies. The genes, known as GDF15 and IGFBP7, are both involved in the development of the placenta and play important roles in early pregnancy and appetite regulation.

Hyperemesis Gravidarum also known as HG, is classified as a severe form of nausea and/or vomiting in pregnancy.
HG is a life threatening pregnancy condition that can kill mother and babies due to dehydration and malnourishment in the mother. Women with HG often experience severe nausea, excessive vomiting, dehydration, and a loss of more than 5% of pre- pregnancy body weight. Some women only have severe nausea that they cannot eat or drink and this is where there is what we call a Greyhound area.
Many experience nutritional deficiencies and need intravenous support.
Women with HG experience difficulty getting along in their daily lives
some require bed rest the whole pregnancy and others spend weeks in hospitalizations. Oftentimes Hyperemesis Gravidarum extends through all three trimesters. Some women feel worse throughout the different trimesters, than others. Mothers with mild to moderate HG that have had their symptoms subsided by the start of the third trimester. There are also women who have experienced HG with one pregnancy and not another. The exact cause behind HG is still unknown. For many HG moms once the pregnancy has ended they often feel immediate relief. There are also many moms who don’t feel completely back to normal for several months , years or forever stuck in the aftermath of hell.
These women still have symptoms from the extreme stress of Hyperemesis Gravidarum.
A lasting impact on their physical health, emotional health, and mental health If you have become pregnant and believe you are suffering from or have been diagnosed with Hyperemesis Gravidarum it’s important to seek treatment ASAP. For those that have suffered in the past may want to try early intervention of treatments, once you find out you are pregnant. It’s important to be on top of and express your medical concerns. Unfortunately many medical professionals are uneducated or believe Hyperemesis Gravidarum is psychosomatic, leaving more women to suffer in silence then treated.
Getting a diagnosis from a medical professional is important in treating HG.
This can be made through doing weight checks to see how much weight has been lost, checking blood work, urine samples, and an examination of the patient, as well as past history. Other women have more severe symptoms that make the diagnoses easier to be made. These can include severe nausea, and vomiting, inability to participate in daily activities, and severe dehydration. Once a diagnosis is made you may seek or be offered treatments and medications. Some of the treatments are standard in terms of HG care such as anti-nausea medication, Zofran, and Intravenous Fluids, Sodium Chloride.
The treatment of Hyperemesis Gravidarum is very complex.
Since HG can cause many different complications due to the extreme nausea and vomiting, it’s important to seek medical attention promptly. There is a broad spectrum of treatments depending on the severity of the HG you are experiencing. Standard treatments for HG are anti-nausea medications such as Zofran and Phenergan. Other medication is reflux medication such as Zantac and Pepcid. Reglan is also another common medication prescribed. Some will need to be administered IV fluids which can be done through a doctor or emergency room. For further treatments, see chapter what are the treatments for HG?
The biggest concern with HG is nutritional deficiencies.
This is It’s important to understand that Hyperemesis Gravidarum can cause multiple different health issues and complications due to the physical stress. The goal is to obtain a healthy effect for mother and fetus. There are multiple ways of accomplishing this in order to minimize the risk of a negative outcome. Many woman fears are that HG or the medications taken during will have a negative outcome on their child. That is a very valid fear and I think most women ponder this question at one point in their pregnancy. It can often times be more detrimental to the fetus to have no nutritional supplementation than it is to take IV fluids and medication.
Again, each person’s Hyperemesis Gravidarum is different, thus the medication and treatments for each person will vary.
There is more likely to be a negative impact on child if the mother suffers from extreme HG that has led to complications. If medical interventions are not taken in a timely matter, this can also increase the chance of the child having complications. It’s important for mother to get adequate nutritional support in order to reduce the chance of complications during pregnancy.
The psychological effect that Hyperemesis Gravidarum takes on mothers is extreme. The constant nausea and vomiting makes one feels helpless. So many mothers suffer from a variety of mental illnesses brought on by HG including depression, anxiety, mood disorders, and other mental illnesses. The most important thing is a support system. Oftentimes this is just one person, a spouse, parent, relative, or friend. Those that don’t have support are more likely to have psychological complications. HG can affect families and friends of individuals suffering. The social impact of HG is stressful as many mothers can’t handle and due simple daily activities. Some people are left completely alone due to the burden HG has on one’s life. It’s important to seek decent psychological help during HG in order to have a healthier less stressful experience. The person needs to take your concerns seriously. It’s important to not blame yourself or the person suffering as HG is out of one’s power.
HG can have a severe impact on one’s finances, relationships and health for mother and baby. .
Many women require medications, medical treatments, and hospitalizations, on top of Obgyn care that is essential to the pregnancy. There are many women that have complications that impact their employment and make the financial burden even more stressful. Many mothers with insurance suffer silently due to complications with coverage. Without insurance HG could easily be detrimental to the mother, child, and couple going through this. Some mothers are forced to have medical abortions due to the severe impact of HG. Future family planning is often limited due to HG’s impact on physical, psychological, and financial aspects of one’s life. The financial burden of HG can become extremely stressful, it’s important to have support during this time.
Morning sickness is a common complication during pregnancy.
These women feel nauseas, generally in the 1st trimester, but subside as pregnancy goes on. With morning sickness women can still eat and drink even with the nausea and vomiting. Morning sickness can be treated with diet and lifestyle modifications such as crackers, ginger ale, sea bands, and other minor outpatient procedures that can be done in the home. These women meet the recommended guidelines for weight. Morning Sickness can cause discomfort but the frequency of vomiting is much less severe than even light Hyperemesis Gravidarum. It’s important to understand the difference between morning sickness and HG. Many mothers are told they have “Acute Morning Sickness”. This is not true and until the media and doctors call it for what it is, HG will still remain as an extremely dangerous complication for women during pregnancy.
There is very little research done on HG. Kate Middleton was one of the first public figures to have Hyperemesis Gravidarum.
The media played a huge part in advocating Kate Middleton’s HG. We need more public figures to come out and talk about HG in order to reach the thousands of women suffering .
Hyperemesis Gravidarum- HG for short. Is a severe life threatening pregnancy sickness, this is NOT morning sickness. HG, "unrelenting, excessive pregnancy-related nausea and/or vomiting that prevents adequate intake of food and fluids." It causes severe dehydration and malnourishment in the mother. HG and morning sickness are not one in the same. Don't let anyone tell you that they are the same as they are NOT! Below we will explain what the difference is and some facts about HG and morning sickness.
Morning sickness, is a symptom of pregnancy that involves nausea or vomiting. Despite the name, nausea or vomiting can occur at any time during the day. Typically these symptoms occur between the 4th and 16th week of pregnancy. About 10% of women still have symptoms after the 20th week of pregnancy.
The type of treatment that is required depends on how ill a woman becomes. Possible treatments might include:
There are many HG groups that offer help with HG. We have groups online to help with ongoing support.
Show off your baby bump with our HGBDATA merchandise.
Will HG go away? If so, when?
Will the medications I take hurt the baby?
Can I survive HG without medication?
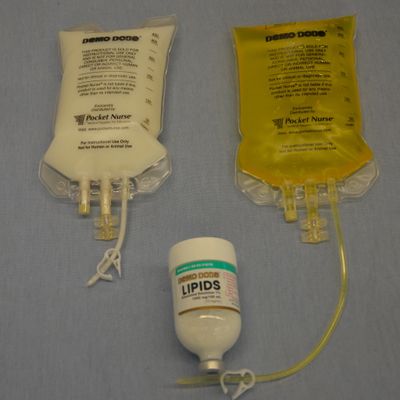
After several weeks of vomiting, you can become very malnourished, yet this may not be realized by health professionals who only see you periodically. This is especially true if you are above your ideal body weight prior to pregnancy. TPPN (Total Peripheral Parenteral Nutrition) or TPN (Total Parenteral Nutrition) may be ordered by your physician to ensure you receive adequate nutrition. TPPN supplies many more nutrients than basic IV fluids. If your health care doctor won't give you TPN you may need to fight for it. Many doctors are misinformed on HG it is very important facts of Nutrition during HG. Do your research.
TPN supplies most of your daily nutritional requirements and is usually given through a catheter called a PICC line placed in the arm, or a central venous line placed in the neck/shoulder area. Local anesthetic is given to minimize pain during the procedure. These catheters are much longer and the end point is in the heart. This allows very concentrated nutrients to be given without damage to the smaller blood vessels of the arms. It is important to note that TPPN/TPN is not a complete formula. Added multivitamins are very important to avoid nutritionally-related complications. Management of HG with Parenteral Nutrition Once you lose over 5% of your pre-pregnancy body weight, nutritional therapies should be discussed, especially if you continue to have significant nausea, vomiting, and weight loss. At a minimum, IV home therapy with added vitamins should be administered after a few weeks of frequent vomiting. Once you lose 8-10% of your body weight or have been vomiting for more than a month, it is imperative that you receive support to replace the many nutrients you have lost and to maintain your hydration. TPPN or TPN is the next choice for ongoing replacement. Dehydration perpetuates the vomiting cycle, as do nutritional deficiencies. If nutritional support is not offered and/or you are not responding to anti-vomiting medications, a second opinion with a specialist may be needed. Nutrition is one of the most challenging and important issues for women with HG. Pregnant women require a variety of nutrients both for their own healing and for the normal development of their unborn child. The baby's requirements for minerals, vitamins, and other nutrients come first and are taken from the mother's bones, organs, tissues, and other storage areas. This can leave the mother depleted very quickly, which can take months, or even years, to correct. These nutrients are also needed to form the placenta, to increase the size of the uterus and breast tissue, and to create amniotic fluid. A mother's blood volume increases by 25–50%, and more fluids, iron, B12, folic acid, zinc and copper, calcium, magnesium, and proteins are needed to support this new blood. Storage levels of most nutrients must be obtained from the diet as well. A nutritional consult may be helpful both during and after pregnancy to ensure she sufficiently rebuilds her nutrient stores, especially before becoming pregnant again.
Nutrition is one of the most challenging and important issues for women with HG. Pregnant women require a variety of nutrients both for their own healing and for the normal development of their unborn child. The baby's requirements for minerals, vitamins, and other nutrients come first and are taken from the mother's bones, organs, tissues, and other storage areas. This can leave the mother depleted very quickly, which can take months, or even years, to correct. These nutrients are also needed to form the placenta, to increase the size of the uterus and breast tissue, and to create amniotic fluid. A mother's blood volume increases by 25–50%, and more fluids, iron, B12, folic acid, zinc and copper, calcium, magnesium, and proteins are needed to support this new blood. Storage levels of most nutrients must be obtained from the diet as well. A nutritional consult may be helpful both during and after pregnancy to ensure she sufficiently rebuilds her nutrient stores, especially before becoming pregnant again. TPN supplies most of you daily nutritional requirements and is usually given through a catheter called a PICC line placed in the arm, or a central venous line placed in the neck/shoulder area. Local anesthetic is given to minimize pain during the procedure. These catheters are much longer and the end point is in the heart. This allows very concentrated nutrients to be given without damage to the smaller blood vessels of the arms. It is important to note that TPPN/TPN is not a complete formula. Added multivitamins are very important to avoid nutritionally-related complications.
It is very typical for mothers with HG to have very strong cravings and aversions that prohibit a well-balanced diet for much of their pregnancies, and these preferences may change frequently until delivery. It may be the smell, texture, appearance or taste that leads to nausea and vomiting. The cause is likely a complex interaction of endocrine (hormone) changes related to pregnancy, nutrient deficiencies, mechanical changes in the body, gastrointestinal dysfunction (e.g. reflux), and changes in neurochemicals. The intensity of cravings and aversions can be very high and trigger repeated bouts of severe nausea and/or vomiting. Thinking about foods, smelling them, or even just seeing food on the television is enough to trigger vomiting for many. She may crave very specific combinations of food characteristics, such as salty and crunchy, or sweet and soft. Entering a grocery store, opening the refrigerator, or even contemplating food preparation are usually intolerable for at least the first trimester. This has significant impact both on her and her family, and is not something she can control. These issues have to be acknowledged, supported and accepted by her family and care providers. It's impossible to fully understand the unusual dietary preferences of HG unless you have experienced it for yourself. Trying to force other foods that do not appeal will typically result in vomiting and greater anxiety for the mother. If a HG mother as for any type of food or drink let her have it. Do not try to force a mother to eat something she doesn't want, you will only make it worse.
While nutritional support is important, some physicians initiate home TPN without having first attempted an adequate trial of antiemetic medications. Serious complications are possible when central venous lines are placed, as well as metabolic and infectious complications. These are usually due to insertion technique, improper care of the IV site or line, or inadequate monitoring of your metabolic and nutritional status with blood tests. However, these problems are estimated to occur in only a small percentage of women with HG, even when TPN is given at home. Before TPN is begun, consideration should be given to aggressive anti-vomiting medications and home IV therapy with vitamins, which do not put you at risk for any life-threatening complications. A growing number of women report that drugs from the serotonin antagonist category (e.g. Zofran, Anzemet, Kytril) have been used in higher doses in their subsequent pregnancies, eliminating the need for TPN and even IV's in some cases. Many physicians (and midwives) are not familiar with the use of these drugs during pregnancy, and are reluctant to offer them in adequate doses (and early enough) to give mothers relief from incessant vomiting. Feel free to refer your health professionals to our site for assistance or find a physician up-to-date on caring for mothers with hyperemesis.After several weeks of vomiting, you can become very malnourished, yet this may not be realized by health professionals who only see you periodically. This is especially true if you are above your ideal body weight prior to pregnancy. TPPN (Total Peripheral Parenteral Nutrition) or TPN (Total Parenteral Nutrition) may be ordered by your physician to ensure you receive adequate nutrition. TPPN supplies many more nutrients than basic IV fluids, and may be given in a regular (peripheral) IV in the arm. However, the IV will typically only last for a few days and will then need to be replaced. TPN supplies most of you daily nutritional requirements and is usually given through a catheter called a PICC line placed in the arm, or a central venous line placed in the neck/shoulder area. Local anesthetic is given to minimize pain during the procedure. These catheters are much longer and the end point is in the heart. This allows very concentrated nutrients to be given without damage to the smaller blood vessels of the arms. It is important to note that TPPN/TPN is not a complete formula. Added multivitamins are very important to avoid nutritionally-related complications.
Once you lose over 5% of your pre-pregnancy body weight, nutritional therapies should be discussed, especially if you continue to have significant nausea, vomiting, and weight loss. At a minimum, IV home therapy with added vitamins should be administered after a few weeks of frequent vomiting. Once you lose 8-10% of your body weight or have been vomiting for more than a month, it is imperative that you receive support to replace the many nutrients you have lost and to maintain your hydration. TPPN or TPN is the next choice for ongoing replacement. Dehydration perpetuates the vomiting cycle, as do nutritional deficiencies. If nutritional support is not offered and/or you are not responding to anti-vomiting medications, a second opinion with a specialist may be needed. See our Referral Network for tips on finding a doctor experienced in treating HG. You may need a friend or spouse to advocate for you while you are sick.

Women with HG may vomit or have severe nausea for months that will leave her exhausted and very depleted. It is imperative that women losing weight rapidly and that are not responding to medications; be given nutritional support via fluids. Research has shown significant nutrient depletion in these women. Vitamins, especially B-vitamins, are depleted very quickly and if not replaced; can worsen her symptoms or put her at risk for life-threatening neurological disorders like Wernicke's Encephalopathy and central pontine myelinolysis (CPM).
At a minimum, mothers requiring hydration should also receive vitamins and electrolytes. Those who continue to lose over 5% of their body weight in the early months should be considered for IV nutrition to protect the mother and unborn child's well-being. Studies show that an inadequate nourished fetus may grow and develop more slowly, have chronic disease in later life, and is more likely to be preterm.
HG mother's are also at greater risk for complications such as pre-eclampsia and postpartum depression. Ironically, nutrition is likely the most prolific topic related to pregnancy, yet when a woman has HG, she is often told malnutrition will not harm her unborn child or herself. Surgical patients are given nutritional therapy typically within one week if they are still unable to eat. If, some doctors seem fit to provide you. It is equally as important to find a knowledgeable HG doctor. Mother's with HG often go weeks or months without food or hydration and are slowly starving and not receiving nutritional support. Research does not support the idea that prolonged starvation is acceptable during pregnancy. These women should be given interventions and better care to promote a healthier outcome for both the mother and child.
Lasting effects can make the aftermath of HG even harder for recovery.
In recent years, research has increased on the use of feedings by either a nasogastric (NG), or a percutaneous endoscopic gastrostomy (PEG) tube as an alternative to parenteral (intravenous) nutrition. This is mostly attributed to decreasing the cost of medical care, and increasing safety. A NG tube is passed through the nose to the stomach or jejunum, and the PEG requires a surgical procedure to implant it through the abdomen into the stomach. Sometimes, the tube will be advanced into the jejunum for added safety and tolerance. This is another form of being able to get nutrition.
What is a PICC line?
A PICC line is a long, soft, flexible tube that is inserted through a vein in the upper arm. PICC stands for Percutaneously Inserted Central Catheter.
When is a PICC line used for HG?
A PICC line is used when a HG mom cannot hold down any fluids food and medications. HG moms needs intravenous medication, such as fluids or hydration during HG or other medical issues . It is important that you know how to take care of your picc line to prevent itching, redness and blisters. Infection rate and blood clots are a huge risk. if you do not care for it right or a nurse that has zero clue what they are doing. You must weigh the benefits over the risk. There are many types of PICC lines out there, they are not all equal.
PICC lines if cared for correctly, can stay in the whole pregnancy. A PICC line can stay in for an extended period of time , unlike a IV in your hand. HG moms need hydration and medication and nutrition, TPN if needed . Medications quickly cause smaller veins to clot off and blow , so they must be delivered into the larger veins closer to the heart. PICC line are used for other health issues, when someone requires frequent blood sampling. The most common uses for a PICC line are for giving antibiotics and chemotherapy through the veins , however moms with HG, it is a good treatment choice for HG moms to get hydration and TPN . The aftermath of poor care during an HG pregnancy can continue and affect you and your baby. after your baby is born.
How is the PICC line placed?
A healthcare professional will place a PICC line in your arm. They will numb your arm. If you feel any pain speak up. If you have POTS Syndrome or Mast cell activation syndrome ask them to tilt the head of the bed. The procedure is done either in a hospital or in an outpatient facility. Using a needle called a guide wire, the professional inserts the PICC line into a vein located in the arm. From there it is threaded into a larger vein near the heart.
Once the catheter is in the correct position, the needle or guide wire is removed and the catheter is left in place. The catheter site is covered with a sterile dressing and the tubing is securely taped to the person's skin. Plastic tubing is connected to the end of the catheter. A Chest x-ray will be done after the PICC line is inserted to check that it is correctly placed. If you are having chest pain after placement or feeling your heart race please let the nurse know. Sometimes the line needs to be pull back 1-3 cm.
PICC line catheters can generally remain in place for days to several months. In some cases, the catheter can remain in place for up to a year.
What type of care does the PICC line require?
The dressing is changed once a week by a healthcare a nurse . If the catheter is not being used continuously, it can be flushed with saline solution to prevent it from clogging. We recommend that you flush it 3-4 times a day. If you have a double lumen flush both sides. Take care of your PICC line, keep it clean and keep a clean cover on it. If it becomes dirty or wet it needs to be changed right away.
What precautions should be taken after a PICC line has been inserted?
The catheter site must be kept dry. The person may bathe or shower as long as the insertion site is protected with a water-resistant covering. Shower covers are not all the same . The limbO cover is the best by far to put on and protect your line from getting wet. If your dressing gets wet you must get it change right away. Please call your home health company and let them know right away.
Do not let anyone check your blood pressure on your PICC line arm.
The PICC line site should be checked every day for signs of infection such as redness, swelling, or pain.
What are the complications associated with a PICC line?
A PICC line is designed to stay in place for many months. However, the catheter can sometimes cause phlebitis, or vein irritation, causing a red streak to appear on the arm.
If the line becomes infected, you may develop a fever, chills, or a rash. some risks associated with the PICC line procedure can include infection, bleeding, blood clot, increased venous thrombosis, pulmonary embolus, breakage of instrumentation during the procedure.
Contact your healthcare professional right away, don't delay. Your doctor should be notified of these, or any other new or worsening symptoms. Your PICC line, left untreated can cause Sepsis that can be life threatening. .
Your PICC line will dangle out of your arm. The tubing coming out needs to be treated as if it was your baby. Do not lift anything more than 1-3 pounds it can dislodged your line. If you have small children do not lift them with that arm, get help if you can.
You PICC line cannot get wet and you need to make sure it's not pulled out and being on the outside of your arm there is that risk ! Your dressing must be changed weekly by a nurse that knows what they are doing! The dressing is changed once a week by a registered nurse. If the catheter is not being used continuously, the nurse will flush the line with saline solution to prevent it from clogging.
PICC lines are easy to care for , please research it so you know the steps of how your arm should be kept clean. If you like to learn more to care for your PICC line check out Mighty Well . This is a great article 7 things not to do with a PICC line.
If you are interested in buying one of their PICCPerfect covers use coupon code: HGBDATA at checkout.
Many moms want to hide there PICC line. They are embarrassed. There are two PICC line covers Starr uses.
What precautions should be taken after a PICC line has been inserted with Hyperemesis Gravidarum?
You must keep the catheter site dry. The person may bathe or shower as long as the insertion site is protected with a water-resistant covering . It must be a Waterproof PICC line Protector is a must. One of our favorites shower covers is called LimbO
The PICC line site should be checked every day for signs of infection, such as redness, swelling, or pain.
What are the complications associated with a PICC line?
A PICC line is designed to stay in place for many months. However, the catheter can sometimes cause phlebitis, or vein irritation. If this occurs, a red streak may appear on the arm, and the healthcare provider needs be notified. Home health care usually have an answering service.
Infection is also possible, but not rare during HG.
The nurse or doctor should also be notified if you develops a fever, chills. If you have extreme itching, blisters please contact your nurse and send us a message for tips and we be glad to help.
Some HG moms get a central line, if a PICC line is not working well. A port or hickman line is a special intravenous line, called a central line. This type of IV is inserted through the chest and threaded into one of the large veins that lie close to the heart. A central line or PICC line can have multiple ports that can be used for drawing blood samples, administering long-term IV therapy like fluids and TPN and medication.
How is the procedure performed?
A central line is inserted under sterile conditions. This m is usually placed in the Trendelenburg position, which means the head is below the level of the heart. The skin is cleansed, and a local anesthetic is injected to make the area numb. A healthcare professional advances the line until it reaches the large vein of the chest. The catheter is then sutured in place, and a sterile dressing is applied.
What happens right after the procedure?
A chest X-ray will be done right away after a central line is inserted to confirm that it is in the right position. The line should not be used until the X-ray is done. A central line can usually stay in place for the whole pregnancy, if cared for properly. Some women need aftermath care and keep them in longer.
What happens later at home?
If you’re going home with the central line, your family will need to learn how to care for the catheter. A visiting nurse can come to the home to help the family with the care at first. The bandage at the insertion site will need to be changed every 3-7 days. The insertion site should also be inspected closely for signs of infection. These signs include redness, warmth, drainage, and swelling.
What are the potential complications after the procedure?
While inserting the line, it is possible to puncture the lung. The catheter may irritate the heart and cause irregular heartbeats, called arrhythmias. Other complications may include:
Air embolism
Bleeding
Blood clot in the tubing
Infection
Migration (your line can be replace if this happens) however having a SecurAcath® can help preserve the line. We highly recommend a SecurAcath to keep your Iv in place.
SecurAcath® is the only Subcutaneous Engineered Stabilization Device (ESD) that meets the 2016 Infusion Therapy Standards of Practice.
The new Standards state Subcutaneous ESDs have been successful in stabilizing PICCs and CVADs
- Patient outcomes and patient and inserter satisfaction have been favorable
The Standards also include a new caution to be aware of the risk of adhesive-related skin injury (MARSI) associated with the use of adhesive-based ESDs
- SecurAcath eliminates MARSI complications of adhesive-based ESDs
Any of these complications may lead to the removal of the central line. Contact us if you have any questions, or if you need help to get in touch with the company of SecurAcath®
How to choose a PICC line cover for your PICC line arm.?
When choosing a PICC line cover it is important to know ahead of time of what type of cover you like. This does not replace the sterile dressing, these go over your dressing to keep it clean and protect your PICC line and tubing.
These go over your dressing to keep it safe. One of our favorite covers and companies who we love at HGBDATA is a cover made by: CareAline is cotton, it soft and great for people who has sensitive skin.
CareAline PICC Sleeve is the original Award Winning and Hospital Approved CareAline PICC Sleeve keeps your infusion lines in place, keeping them off of your skin. Their products keep lines off of your skin because lines are fed through a specially designed, patented buttonhole. This eliminates the need for irritating tape to hold the tube and cap in place when you are not being treated. There is a pocket that keeps your caps safe and secure while not in use, and a patented privacy cover to keep everything hidden. If you are interested in buying a PICC line cover instead of using mesh or a old sock. We have two companies that have outstanding products to cover your PICC line and highly recommend with the Starr's seal of approval .
CareAline and PICCPerfect both are great covers depending on what type of fabric you prefer. Use coupon code : HGBDATA at checkout for a discount for all of our HG moms who need to feel better to lift their self esteem.
PICCPerfect
The PICCPerfect® 2.0 PICC Line Cover protects and covers your PICC Line and helps prevent pulling and/or displacement. Its unique fold-over design and double access openings will allow you to do your medical treatment without exposing your PICC Line insertion site. Your PICC does not have to touch your skin!
Use coupon code: HGBDATA at checkout for both websites .
Having IV fluids at home or TPN and medications such as a Zofran pump can be life saving to stay out of the hospital . A nurse can come to your home to put your IV in every few days if your doctor will not do a PICC Line, It's important to know your options.
Copyright© 2010- 2025 HG Before During And The Aftermath/HGBDATA, HG HG Activist Life, and All affiliated websites, blogs. vlogs,social media platforms, books promotional content, logos, slogon, ribbon colors of blue, red, purple (i.e) are copyrighed by us and in common law tradmark. Please reach out to us for permission . YOU MAY SHARE OUR WEBSITE, VIDEOS, VLOGS,BLOGS ONLINE OR TV.. You may list us as a resource, to add to your list, and for educating purposes. YOU MAY NOT brand it with your own company info
( i.e) if you are unsure what this means please contact us, we would love to collaborate with you. We give permission to share our content on your social media platforms and TV. We ask for you to link to our website to credit the source. DISCLAIMER: HG before during and the aftermath does not intend to dispense medical advice and should not be considered medical advice or counsel. If you have a question about your health or the health of your child please consult your physician. *If you need to speak with an HG Crisis Volunteer, we offer support and understanding. We will help you advocate, for yourself and or your baby. Always speak with your doctor.*
We are not giving medical advice however we will educate you on HG and the aftermath. By helping you learn to advocate for you and your baby/ child . The stories and information here are educational and of personal opinion only and should not be used as a substitute for medical help. The information is to educate yourself . Knowledge is power and the key to fight for your care. Because no one else will.
You can contact us for questions or help with HG and for a personal HG support sister, advocating, and help with explaining to your doctor about HG. We want you to know you are never alone. We are here for mothers with HG and in the aftermath of HG.
☆We work together and support the HER Foundation in everything they do for HG☆
PLEASE NOTE: Most Information on this website is courtesy from the HER Foundation. http://www.helpher.org/ If you like to help fun education and research for HG, please visit Hyperemesis.òrg and help fundraise to excel their research. All fundraising HGBDATA does is for HER and all proceeds go to the HER FOUNDATION. *in less otherwise stated differently *
*WE GIVE PERMISSION FOR THE MEDIA TO SHARE OUR CONTENT ON THE NEWS,VLOGS, ARTICLES. Would love to help more such as interview with you .
TO PROMOTE AWARENESS